In the ever-evolving landscape of patient care, innovations such as High-Flow Nasal Cannula (HFNC) have emerged as a game-changer, particularly in intensive care units (ICUs) and emergency departments (EDs). This noninvasive ventilation method has shown its potential to significantly impact patient outcomes compared to conventional oxygen therapy. In this article, we delve into the mechanisms of action, clinical studies, and physiological effects of HFNC, highlighting its relevance in treating critically ill patients, including those with acute hypoxemic respiratory failure and acute respiratory distress syndrome.
The Basics of High-Flow Nasal Cannula
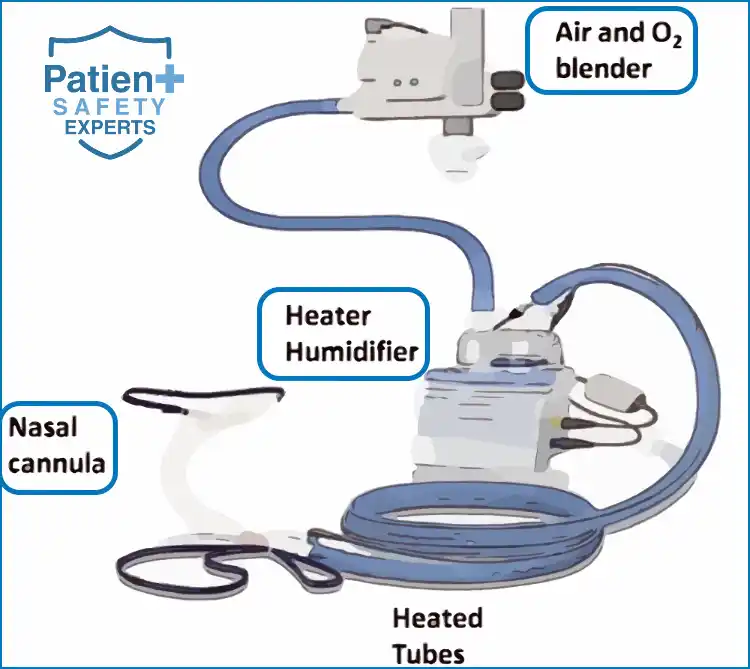
HFNC is an innovative respiratory support system that delivers high-flow oxygen through nasal prongs to adult patients. Unlike traditional oxygen delivery methods such as standard nasal cannulas or face masks, HFNC provides high-flow oxygen blended with room air using an oxygen blender.
Key Components
- Oxygen Blender: The oxygen blender allows precise control over the fraction of inspired oxygen (FiO2), enabling tailored therapy for patients. It is a critical component of HFNC’s efficacy.
- Heated Humidifier: HFNC incorporates a heated humidifier to provide warm and humidified gas to patients. This maintains airway humidity, ensuring patient comfort and reducing the risk of drying and irritation.
- High Flow Rates: HFNC delivers high flow rates, typically ranging from 20 to 60 liters per minute (L/min). These high flow rates help wash out the anatomical dead space and reduce the work of breathing.
High Flow Nasal Cannula Mechanisms of Action
- Optimal Oxygenation: HFNC ensures patients receive an optimal oxygen level, improving oxygenation. This is crucial in managing critically ill patients.
- Positive End-Expiratory Pressure (PEEP): HFNC can create slight positive pressure in the oropharynx
- Reduction in Work of Breathing: HFNC offers continuous positive airway pressure (CPAP), which reduces the work of breathing. This is particularly beneficial for patients in respiratory distress.
- Washout of Dead Space: The high flow rates effectively wash out the anatomical dead space, minimizing the rebreathing of exhaled carbon dioxide (CO2) and enhancing ventilation.
Enhanced Oxygenation
High Flow Nasal Cannula (HFNC) offers a unique advantage by delivering high and consistent fractions of inspired oxygen (FiO2). This improved oxygenation is due to the capability of HFNC to provide a flow rate that meets or exceeds the patient’s peak inspiratory flow rate, leading to:
- Consistent FiO2: Reduced entrainment of room air, resulting in a stable and predictable FiO2.
- High Flow Rates: Allows delivery of flow rates up to 60 L/min, ensuring the set FiO2 is maintained.
Positive End-Expiratory Pressure (PEEP)
While not a replacement for the PEEP delivered by mechanical ventilators, the HFNC does create a slight positive pressure in the oropharynx:
- Alveolar Recruitment: Helps in keeping alveoli open, potentially improving oxygenation.
- Counterbalance Intrinsic PEEP: Can counteract auto-PEEP in chronic obstructive pulmonary disease (COPD) patients.
Decreased Work of Breathing
HFNC has shown to assist in decreasing the work of breathing in some patients:
- Meeting Inspiratory Demand: By matching or exceeding the patient’s peak inspiratory flow rate.
- Enhanced Carbon Dioxide (CO2) Washout: Efficient removal of CO2 from the anatomical dead space.
Optimal Humidification and Warming
HFNC systems typically include an active humidifier which provides several physiological advantages:
- Maintains Mucociliary Function: Optimal humidification ensures the integrity of the mucociliary system.
- Prevents Mucosal Drying: Reduces the discomfort often seen with traditional oxygen therapies.
- Warming: Warm gases mimic physiological conditions, improving comfort and aiding in mucosal function.
Reduced Anatomical Dead Space
The high flow rates provided by HFNC help in:
- Dilution of Fresh Gas: With the existing alveolar gas, improving the efficiency of gas exchange.
- CO2 Washout: From the upper airway, reducing rebreathing of CO2.
Clinical Studies and Evidence for High-Flow Nasal Cannula
HFNC therapy has gained recognition through numerous clinical studies and randomized controlled trials. These studies have shed light on its efficacy in various clinical settings, particularly in patients with acute respiratory failure and other critical conditions.
Primary Outcomes
- Intubation Rate: Several studies have reported a significant decrease in the intubation rate among patients treated with HFNC compared to those on conventional oxygen therapy. This is particularly noteworthy in the context of avoiding invasive procedures like endotracheal intubation.
- Mortality Rate: While results may vary, some clinical trials have demonstrated a decrease in mortality rates in patients who received HFNC therapy. This underscores its potential to improve patient outcomes.
- Clinical Improvement: Patients treated with HFNC have shown significant improvements in vital signs, including heart rate and oxygen saturation. These improvements are vital indicators of patient well-being.
Clinical Settings
HFNC has found utility in various clinical settings, including:
- ICUs: HFNC is often considered a first-line treatment for patients with acute respiratory distress syndrome (ARDS), chronic obstructive pulmonary disease (COPD), heart failure, and septic shock.
- EDs: In the emergency department, HFNC therapy can rapidly provide high-flow oxygen to patients, especially those with acute hypoxemic respiratory failure.
- Acuity Adaptable Units: HFNC is a valuable tool for delivering high-flow oxygen therapy, providing adequate oxygenation even in patients with high oxygen demands.
Patient Comfort and Adverse Effects
Patient comfort is a paramount concern in healthcare, and HFNC excels in this regard. The warm and humidified air delivered by HFNC enhances comfort and minimizes nasal irritation, a common concern with traditional nasal cannulas.
While HFNC is generally well-tolerated, healthcare providers must remain vigilant for potential adverse effects, such as airway resistance. Monitoring patients through pulse oximetry and regular assessment of respiratory rate is essential to ensure the therapy’s safety and effectiveness.
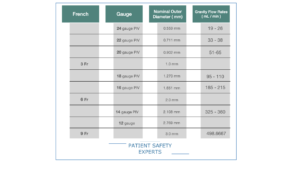
Flow Rates in High Flow Nasal Cannula (HFNC) and Titrating Guidelines
The choice of flow rates largely depends on patient needs, comfort, and the specific clinical scenario.
Table: HFNC Flow Rate Guidelines and Titration
| Patient Group | Initial Flow Rate (L/min) | Titration Guidelines |
|---|---|---|
| Neonates | 4-6 | Increase by 1-2 L/min as required, ensuring comfort and desired oxygenation levels. Monitor for signs of nasal trauma. |
| Infants | 6-8 | Gradually increase in increments of 1-2 L/min, ensuring patient comfort and aiming for optimal oxygenation. |
| Children | 8-15 | Titrate up by 2-4 L/min, observing for signs of discomfort or excessive PEEP. Aim for satisfactory oxygenation levels. |
| Adults | 30-45 | Begin at a lower range and increase by 5-10 L/min as necessary. Maximum can go up to 60 L/min, depending on patient tolerance and oxygenation goals. |
Titrating Guidelines:
- Start Low: Always start with a flow rate on the lower end of the recommended range for the specific patient group. This ensures patient comfort and reduces potential complications.
- Assess Patient Comfort: The patient’s comfort is paramount. If they seem uncomfortable, it may be necessary to reduce the flow slightly. Conversely, if they remain hypoxemic or show signs of increased work of breathing, increasing the flow may be beneficial.
- Target Oxygenation: Regularly monitor the patient’s oxygen saturation (SpO2) and titrate the flow rate to achieve the target SpO2 set by the clinician.
- Limit Maximum Flow: Especially in adults, while HFNC can deliver up to 60 L/min, it’s essential to ensure the patient is comfortable and there’s no evidence of complications like barotrauma.
- Re-evaluate Regularly: Continuously assess the patient’s clinical status. If they are not showing signs of improvement or if their condition is deteriorating, reconsider the therapy and think about alternatives or escalations in care.
- Weaning: Once the patient shows signs of improvement, consider gradually reducing the flow rate, ensuring that the oxygenation target is still met.
Indications for High Flow Nasal Cannula (HFNC) Use in Critical Care
| Indication | Details |
|---|---|
| Acute hypoxemic respiratory failure | Suitable for patients who fail to respond to conventional oxygen therapy. |
| Acute heart failure | To improve oxygenation and reduce the work of breathing. |
| Post-extubation | Reduces the risk of reintubation in selected patients. |
| Pre-intubation oxygenation | Can be used as a bridge to intubation or other advanced oxygenation techniques. |
Comparing HFNC with Other Oxygenation Methods
| Method | Advantages | Disadvantages |
|---|---|---|
| HFNC | – Delivers warm and humidified oxygen – Reduces work of breathing – Provides low-level PEEP | – Not suitable for severe hypoxemia – Requires close monitoring |
| Standard Nasal Cannula | – Simple to use – Easily available | – Limited to low flow rates – Can cause nasal dryness |
| Non-invasive Ventilation (NIV) | – Provides positive pressure support – Useful in hypercapnic respiratory failure | – May cause facial discomfort – Needs expertise to setup |
| Mechanical Ventilation | – Suitable for severe respiratory failures – Offers full control over breathing parameters | – Invasive – Risk of ventilator-associated pneumonia |
Breath Easy: The HFNC Quiz Challenge
Question
Your answer:
Correct answer:
Your Answers
Benefits and Limitations of HFNC in Critical Care
Benefits
- Improved Oxygenation: Achieves higher levels of FiO2 compared to conventional oxygen therapies.
- Humidification: Provides warmed and humidified oxygen, enhancing comfort.
- Positive End-Expiratory Pressure (PEEP): Creates a slight positive pressure, aiding alveolar recruitment.
- Reduced Nasal Dryness: Lessens discomfort due to constant airflow.
Limitations
- Limited to Moderate Acuity: Not suitable for patients with severe hypoxemia requiring intubation.
- Requires Monitoring: Flow and oxygen settings need regular adjustments.
- Potential Delay: In transitioning to invasive ventilation when necessary.
- Power Dependency: Needs a continuous power source for operation.
Learn more about safe central line placement techniques.
HFNC in the Age of COVID-19
The COVID-19 pandemic has placed HFNC in the spotlight, particularly in managing critically ill COVID-19 patients. Clinical studies have explored its role in delivering high-flow oxygen to COVID-19 patients, with promising results. HFNC therapy has been a crucial tool in addressing the hypoxemia challenges the virus poses and helping patients avoid intubation.
Maintenance and Safety Measures for HFNC in Critical Care
Maintenance
- Routine Cleaning: Regularly clean and disinfect all components.
- Filter Replacement: Change filters as recommended by the manufacturer.
- Flow and Oxygen Monitoring: Continuously monitor and adjust based on patient’s needs.
Safety Measures
- Ensure Correct Size: The nasal prongs should fit comfortably without causing pressure injuries.
- Monitor for Complications, Such as nasal dryness, epistaxis, or gastric distension.
- Avoid Delay in Intubation: Recognize when HFNC is insufficient and transition to invasive methods if needed.
- Patient Supervision: Continuously monitor the patient for any signs of deterioration.
Conclusion
High-Flow Nasal Cannula has emerged as a beacon of hope in patient care, offering a noninvasive yet highly effective means of oxygen delivery. Its ability to improve oxygenation, reduce the work of breathing, and enhance patient comfort has made it a first-line therapy in critical settings.
As healthcare providers continue to embrace this innovative respiratory support system, ongoing medical education and awareness of its potential are vital. The wealth of evidence from clinical studies underscores HFNC’s importance in managing acute hypoxemic respiratory failure, acute respiratory distress syndrome, and other critical conditions.
In the journey toward enhanced patient safety and well-being, HFNC stands as a testament to the power of medical innovation and its positive impact on patient care. Its continuous evolution and integration into clinical practice continue to save lives and improve outcomes for patients, especially those in their most critical moments.